An LCGB hosted workshop:
Infant and Young Child Feeding in Emergencies: working with refugee families in Europe 2016
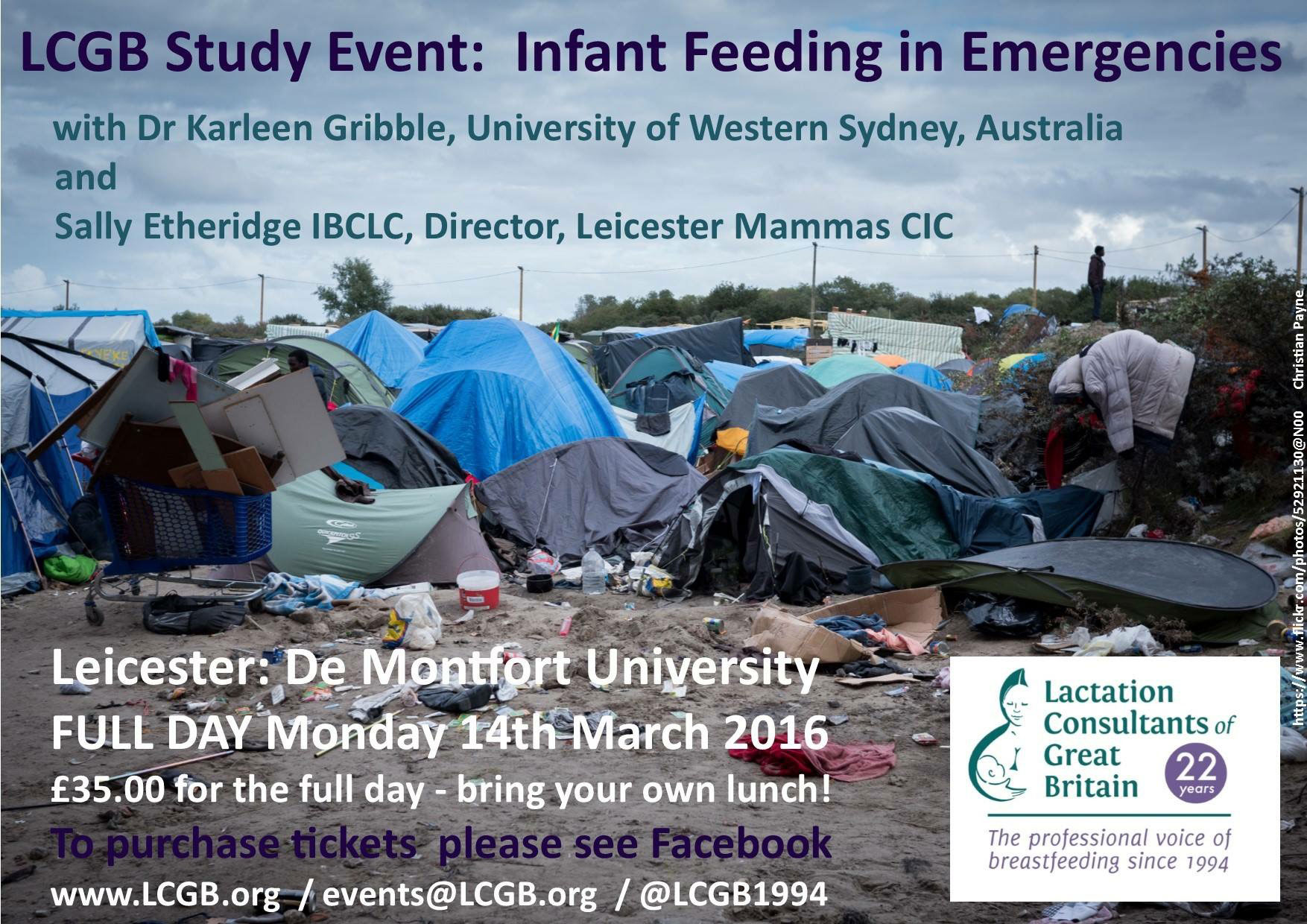
In emergencies, infants and children under the age of 2 are the most vulnerable. The current refugee crisis has displaced millions of people and brought tens of thousands of children and pregnant women to Europe (over 88K children in 2016 alone according to UNHCR figures). Even in Europe, whether they are in transit, or in a refugee camp, these children are incredibly vulnerable.
The response to the refugee crisis in Europe has proved different to previous emergencies, not only through the sheer numbers of people, but with the number of countries involved, the lack of a coordinated response and the involvement of large numbers of untrained volunteers. This has all contributed to especial risks with regard to infant feeding.
Dr Karleen Gribble PhD is an Adjunct Associate Professor at the School of Nursing and Midwifery of the University of West Sydney, Australia and an Australian Breastfeeding Association Community Educator and Breastfeeding Counsellor. She is also one of only two individual members of the Infant Feeding in Emergencies (IFE) Core Group.
The IFE Core Group is an international community of practice around infant and young child feeding in emergencies (IYCF-E) that functions as an interagency collaboration, with members including the likes of UNICEF, ENN (Emergency Nutrition Network), Save the Children, International Rescue Committee, etc. The IFE Core Group’s work to date has centred on development of policy guidance and capacity building tools, capturing and learning from what happens in emergency response with regard to infant and young child feeding and promoting policy and practice change in the context of preparedness and response.
In March, Karleen held workshops on Infant and Young Child Feeding in Emergencies (IYCF-E) in London, Manchester and Paris, aimed at volunteers working with refugee families in Europe.
I’m a trainee breastfeeding counsellor with the Association of Breastfeeding Mothers (ABM) and a Doula UK registered doula. I have become increasingly interested in IYCF-E since starting to volunteer to help with the current refugee crisis in September 2015 and am a member of the Infant Feeding Support for Refugee Children group which developed resources for the SafelyFed campaign. I attended the London workshop, which was my first formal training in IYCF-E, although I had been learning ‘on the job’ for 6 months previously.
The London workshop packed a lot in one day, especially for those attendees without any prior knowledge of IYCF-E recommendations and practice. The workshop attendees varied from infant feeding specialist midwives to breastfeeding counsellors to mothers. Some had experience of working with refugees, or in emergency situations, but many didn’t.
 International Recommendations
International Recommendations
After introducing herself and the IFE Core Group, Karleen looked at what the recommendations are and why these are the recommendations.
The Global Strategy for Infant and Young Child Feeding states that:
Infants and children are among the most vulnerable victims of natural or human-induced emergencies. Interrupted breastfeeding and inappropriate complementary feeding heighten the risk of malnutrition, illness and mortality. Uncontrolled distribution of breastmilk substitutes, for example in refugee settings, can lead to early and unnecessary cessation of breastfeeding. For the vast majority of infants emphasis should be on protecting, promoting and supporting breastfeeding and ensuring timely, safe and appropriate complementary feeding. There will always be a small number of infants who have to be fed on breast-milk substitutes. Suitable substitutes, procured, distributed and fed safely as part of the regular inventory of foods and medicines, should be provided.
The impact of infant feeding on child health in wealthy contexts was discussed and compared to the impact in resource poor contexts. Looking at the difference between morbidity and mortality rates in resource poor environments (less developed countries, but not emergencies) shows a shocking difference: babies under 2 months are nearly 6 times more likely to die if they are not breastfed. This increase in risk decreases as a baby gets older, but for babies 9-11 months old, they are still 1.3 times more likely to die if not breastfed.
How the environment changes when an emergency occurs was discussed. Many things we take for granted – having access to clean water, being able to wash up utensils and keep ourselves clean, etc – are simply not possible in emergencies. The different challenges faced by breastfeeding mothers and carers of formula fed babies in emergencies were brainstormed in group work.
Karleen covered past emergencies around the world that provided unfortunate education on the importance of IYCF-E. One of these was Botswana, which suffered extreme floods in 2005/2006. During this emergency, hospitals were overwhelmed with sick children: there were over 500 deaths in hospitals, of which 96% were children and infants under 2 years. Formula fed babies were 30 times more likely to need hospital treatment and were more likely to die: in one hospital cohort of 153 young children, 93% were not breastfed and 33 children died, all of whom were fed formula (32/33 being not breastfed at all). In one village, 30% of those babies fed formula died, none breastfed. The life-saving impact of breastfeeding in emergencies is clear.
Resources and Assessments
The resources available to support IYCF-E were covered. The following guidance documents are the references in this field:
- The Global Strategy for Infant and Young Child Feeding, jointly developed by WHO and UNICEF.
- The WHO International Code of Marketing of Breast-milk Substitutes.
- The Sphere Project: Humanitarian Charter and Minimum Standards in Humanitarian Response (also called the ‘Sphere handbook’ or ‘green book’), which is the recognised standard to work to for all organisations working in humanitarian response.
- Infant and Young Child Feeding in Emergencies: Operational Guidance for Emergency Relief Staff and Programme Managers (also known as the ‘yellow book’), which is referred to by the Sphere handbook.
- The Interim Operational Considerations for the feeding support of Infants and Young Children under 2 years of age in refugee and migrant transit settings in Europe (version 1.0 issued 1st October 2015), which was specific to the moving crisis in Europe and is in place while a more detailed programmatic guidance is in development by the IFE Core Group.
Assessments are key in properly supporting IYCF-E. Without some basic knowledge, how can you know what support needs to be available in any one place or how to best support a mother or carer of an infant or young child? A basic assessment of a situation, such as a refugee camp, should include:
- How many infants and young children of different ages?
- What proportion are fully breastfed, mixed fed, fully formula fed, fed other foods at less than 6 months or fed complementary foods at 6+ months?
- Changes in feeding practices
- How many separated or motherless infants?
- Use of bottles
- Distribution/availability of infant formula, other milks and other baby foods
- How many pregnant and lactating women?
- Morbidity and mortality causes and rates?
Supporting IYCF-E
Supporting breastfeeding mothers
Group work was used in the workshop to brainstorm what breastfeeding women need in an emergency. This includes:
- Material support: priority access to food, water, accommodation and other resources so that they can prioritise breastfeeding.
- Health services that support breastfeeding: this was illustrated by pictures of a injured mother following the Nepal earthquake, lying in a makeshift hospital, breastfeeding her baby. It is very easy for health services, even in developed countries without an emergency, to put up barriers to breastfeeding for women who need medical assistance.
- Protection from donations, of formula, but also bottles, baby foods and other products covered under the WHO Code.
Protecting from formula donations
The impact of formula donations was discussed in depth and this is a real issue in this refugee crisis in Europe and elsewhere. Formula distributions are often widespread and indiscriminate in emergencies – one study which Karleen mentioned found that over 70% of parents/carers of all babies under 6 months had been given formula, regardless of how baby is fed. The prevalence of formula distributions, from all kinds of sources, was illustrated by images of formula donations from national armies and individuals, Karleen mentioned having to, in her role as part of the IFE Core Group, intervene to stop some of these inappropriate and unhelpful donations.
When organisations and groups have freely given formula donations, they want to give it out and are not careful to only give it out when absolutely needed, as they would be when paying for it. I have seen this myself in Greece and France: one medic tent at a transit point in Lesbos was giving a tin of powdered formula to every family with a baby they saw, without any assessment of whether that baby was fully formula fed, and sometimes without even clean water and a clean utensil to give the formula in.
Studies have repeatedly shown that, if formula donations are given, then more families will use formula and children given formula donations are twice as likely to need medical attention for diarrhoea as those who did not receive formula. The impact can also be long-lasting. Following the 1988 Armenian earthquake there was an influx of aid and inappropriate distribution of infant formula resulted in an immediate and extended decrease in breastfeeding rates: from 64% of babies exclusively breastfed to 4 months, down to 59% 2 years on and down to 20% 6 years on from the disaster. It took 13 years for breastfeeding rates in Armenia to return to pre-disaster levels.
Formula donations are often the wrong type of formula– powdered formulas, unneeded and unwanted follow-on formulas, or specialist formulas – given in the wrong places, they may be out of date or unsuitable for other reasons, such as having instructions and safety warnings in a language the parents or carers cannot read.
Formula donations in emergencies are often not just given to those parents and carers who genuinely need formula. Some of the photos used to illustrate this section included aid workers demonstrating bottles use to rooms of women, including some breastfeeding in the actual photo.
The message for volunteers and NGOs was clear: don’t accept donations, don’t solicit donations, don’t distribute donations. Do discourage donations and do collect and quarantine them on the ground. Many will be unsuitable for use anyway.
Some of the many complex reasons why breastfeeding mothers request and use donated infant formula were discussed, including:
- Belief that the emergency has adversely affected their milk. The myth that stress affects milk supply is widespread amongst parents, volunteers, doctors and NGOs without appropriate IYCF-E training.
- Aspiration to bottle feed. In many developing countries and in emergencies, formula becomes disproportionally expensive. If you are used to thinking that formula is something wealthy people use, you have experienced marketing that formula is good for your child, or you have come from an emergency situation where formula is fetching inflated prices (one tin can be $200+ in parts of Syria), then you take formula when it is freely offered to you.
- Seeking security, either in a ‘in case we need it’ mentality or to simply sell on and provide an income.
- Formula feeding is normal. In many parts of the Middle East, for example, while breastfeeding rates are relatively high, so are formula usage rates – a large proportion of babies are mix-fed. Many of these mothers do not realise that exclusively breastfeeding is a possibility or how great an impact that would have on reducing their child’s risk of illness and death.
What to do to help mothers who believe they need formula milk was discussed in the workshop, along with what can be done to help mothers to feed their babies only breastmilk. Breastfeeding counselling skills are vital and are what is lacking in many scenarios. The breastfeeding counsellor:- builds the mother’s confidence, that she can breastfeed and that she has enough milk; gives accurate information to correct misconceptions and answers questions; makes sure the mother is supported in other ways, for example with extra food or by being connected with other mothers. With breastfeeding counselling skills, you do not dictate to mothers, and you do not promote a course they may well not be happy with, by either reaffirming myths or pushing formula as an alternative. Sadly both of these mistakes are common amongst both healthcare professionals without IYCF-E training and lay volunteers in the European refugee crisis.
The importance of breastfeeding counselling
Karleen went into some depth, including case studies and a role play, to illustrate what breastfeeding counselling is and is not, covering: the theoretical foundations of counselling practice (unconditional positive regard, congruence, creating emotional safety), the theoretical foundations of counselling process (empathetic understanding, understanding the mother’s experience and validating, accepting and valuing that experience), key counselling skills, exploratory questions, clarifying questions, offering information not instruction, offering appropriate reassurance and then offering suggestions and helping to make a plan.
Support for breastfeeding mothers is needed because everywhere in the world, mothers’ concerns about their infants are the same. They worry about their baby getting enough milk. They feed their babies other foods because they think their milk is not good enough, or they don’t have enough milk, in an attempt to solve problems, or because they have to work. They don’t understand the ramifications of feeding formula or they feel that they don’t have any choice. They do not necessarily need to feed infant formula. And in emergencies, there are added pressures.
Karleen emphasised that it is crucial that volunteers and aid workers realise that a request for formula does NOT necessarily indicate a real need for formula. Also, giving a breastfeeding mother formula is NOT kind, as many people without training assume it is.
Supporting carers of formula fed infants
Individual assessment is required to support carers of formula fed infants in emergencies. First, an infant feeding supporter needs to identify if breastfeed is possible. If alternatives are needed, considering options of obtaining breastmilk should be the next step.
Milk sharing in Muslim cultures is often misunderstood. Whilst different nationalities, groups and individuals have different takes on it, the general view is that breastfeeding is considered important in Muslim culture, and breastfeeding a child who is not your own creates a bond: ‘milk kinship’. Children who breastfeed from the same woman, even if she is not their biological mother, are considered to be related. So milk sharing from unknown strangers, or using milk banks where milk from different women is mixed, is often not acceptable. However, that does not mean that milk sharing is not an option, just that it is given greater weight than in might be in non-Muslim cultures.
Supporting mothers who are mixed feeding is an important consideration in this crisis because there are very high rates of mixed feeding in refugees from the Middle East. The guidance is clear that these mothers should be encouraged and supported to drop the formula top-ups and move to exclusive breastfeeding. However, without proper assessment, these families are often assumed to be fully formula-feeding and are encouraged to feed more formula.
When supporting families or carers of motherless infants, consider what the options are for obtaining breastmilk. If they are with other family members, aunts and even grandmothers may be able to take on feeding the motherless infants. There may be other options for wet-nursing or the use of donated milk, depending on circumstances and cultural practices. If they cannot be breastfed, or fed human milk, then safe formula feeding must be supported. This can include being aware that carers may be unused to using formula and may be unaware of how to do so safely, even without emergency considerations.
When supporting fully formula fed infants, it is important to find out how long it has been since the mother stopped breastfeeding, what her ability and motivation to relactate is and whether a wet nurse is available. Supporting safe formula feeding is needed, and Karleen commented that, for many people working in IYCF-E, they come from a breastfeeding support background, but end up spending more time supporting formula feeding!
Relactation is an option often not mentioned to mothers and carers or considered a possibility by aid workers and volunteers. Relactating (restarting lactation having breastfed before) is a simple process of using frequent suckling or nipple stimulation (e.g. with a breast pump) to slowly build supply. Galactagogic medications are not needed and women can relactate even after a gap of many years since they last breastfed.
If the mother breastfeeding is not an option, then wet nursing should be considered. If they are in a camp, than another mother might be willing, especially if there are incentives, such as additional food packages. It is far from unknown for aid workers and volunteers, even police women, to breastfeed other babies in emergencies. Combining wet-nursing and relactation can be an option for some babies.
Minimising the risks of formula feeding is critical in IYCF-E work. Individual assessment of need is essential and then ensuring that the necessary resources are provided: infant formula, feeding implements, preparation and storage resources, clean water, education and health support. Karleen emphasised that it is very difficult to do well and supporting safe formula feeding in emergencies is very difficult.
The guidance all recommends that bottles are not used in emergencies (cups are recommended for all babies not breastfed) because they are impossible to get properly clean, without ready access to unlimited hot water, washing up and sterilising facilities. This particular issue was profoundly illustrated by the photo of a bottle, handed in to a lactation consultant in a camp in Lebanon as part of a cup-for-bottle exchange. The following day, the bottle had maggots growing in it. Cups and spoons are recommended for all babies not breastfed, and ‘bottle exchanges’ have been successfully run in some camps. ‘Disposable’ bottles are not recommended because they can be reused by desperate families, even if it means cutting a hole in the bottle.
The importance of using ready to feed infant formula was discussed, along with the problems that still exist (such as increased risk of infection and the need to have clean utensils to get the formula into babies) and the problems it creates. Getting hold of suitable supplies can be very hard for NGOs. UNICEF and other large NGOs have in the past got together to specifically order unbranded ring-pull cans of RTF formula with instructions in the required languages, but there is no ongoing supply chain of this kind of product for NGOs. They usually have to order branded formula and may then have to relabel packages to have instructions in the required languages.
Breastfeeding women need to be protected alongside supporting reduced-risk formula feeding. Proper assessment is always needed and incentives for breastfeeding mothers should be considered. Otherwise it is easy for a situation to develop where formula feeding carers get given ‘stuff’ while breastfeeding mothers do not, increasing the likelihood they will take formula anyway. Maternal care packs and extra food distribution for breastfeeding mothers are two options that can help.
Supporting formula feeding for families on the move is especially difficult and is partly why the ‘Interim Considerations for the feeding support of Infants and Young Children under 2 years of age in refugee and migrant transit settings in Europe’ were developed. Not only can you have a short amount of time with families in transit, but there may well be difficulties ensuring they have an ongoing supply of suitable formula and they may be less willing to change to cup feeding, whilst simultaneously being completely unable to clean anything. The Transit guidelines (the ‘Feeding Your Baby While You Travel’ flyer developed by the Infant Feeding Support for Refugee Children group) recognise how difficult the situation is and has the goal of harm minimisation.
 The Psychological Impact
The Psychological Impact
Psychosocial first aid
A consideration of psychosocial first aid is a necessary part of supporting IYCF-E. Psychosocial first aid is a humane response to someone who is suffering and may need support. The three steps are: look; listen; link.
Look
- Check for safety
- Look for infants and young children and their caregivers with obvious basic needs
- Look for infants and young children and caregivers with serious distress reactions
The greatest threat to an infant is to be abandoned, then to have non-responsive care. Babies are not very aware of the environment, and experience stress through their caregiver. Babies do not exist on their own, their brains can only develop in relationship with a caregiver. Stress decreases the ability see what baby needs and to respond and a stressed caregiver can transmit stress to his/her child through being unresponsive. Parents and caregivers in stressful situations can also continue to be responsive to the children despite the environment and this is what babies and young children need most.
Babies and young children show stress through: body language; clinging to parents; regression; crying and being irritable; being afraid; changes in sleep and eating patterns.
Being able to identify vulnerable infants and strength in caregivers is important. A mother reacting with touching, just generally being engaged somehow, with a baby is being responsive. A mother who is physically or emotionally distant will struggle to respond to her child. Mothers who have experienced trauma and great stress, as most refugees have, can become distant or experience flashbacks, so it’s like they are ‘not there’ mentally which is traumatic for babies, even if their physical needs are being met.
Listen
- Approach caregivers who may need support
- Ask about their concerns
- Listen to them and help them to feel calm
Link
- Help caregivers to address basic needs and access services
- Find solutions to problems
- Provide information
What does psychosocial support look like in IYCF-E
For mothers of breastfed infants:
- Keep close together
- Skin-to-skin
- Reduced stress
- Support from others
- Referral as needed
- Breastfeeding (support)
For caregivers of formula fed infants:
- Keep close together
- Skin-to-skin
- Reduced stress
- Support from others
- Referral
It is very important that all volunteers recognise that separating a mother/caregiver and baby is not helpful and may be psychologically harmful for both. Examples given included volunteers dubbed ‘baby snatchers’ for the way they would take babies away from mothers and bathe, clothe and hug them without the mother’s involvement.
Breastfeeding supports both maternal and infant psychological wellbeing. It helps mothers to care sensitively for their babies (through the hormones oxytocin, prolactin & cholecystokinin and proximity). Babies not breastfed are more likely to be abandoned, more likely to be abused and neglected (though of course not all will be!). Protecting the physical safety and emotional development of infants should include supporting breastfeeding
Educate and communicate
Karleen ended the workshop by discussing the importance of education and communication around IYCF-E, challenging organisational and individual ideas about what will help and what won’t help.
Training is key for all volunteers. Online training in IYCF-E is available from UNICEF and the Emergency Nutrition Network (ENN). Details of these and other resources are available on safelyfed.org.
Received with grateful thanks from workshop delegate Lindsey Middlemiss, who is a doula, and also helps with antenatal preparation and infant feeding support.

